7 Important Tips for NICU Parents

At my 35-week ultrasound, they discovered my baby had IUGR, intra-uterine growth restriction. She was 4 lbs, which put her in the 4th percentile for weight.
Essentially, my placenta was like a clogged pipe and she wasn’t getting the nutrients she needed. They began twice-a-week fetal monitoring and told me I’d likely be induced early, because in these cases, it’s better for babies to grow on the outside rather than struggle on the inside.
At my 36-week appointment, they took my blood pressure: no good. It had been high all along and now it was over 140. I had to go to the ER immediately for more testing.
Gulp.
I was nervous but my OB reminded me that even if they had to induce me that day, the baby was over 36 weeks old and should be fine.
At the ER, my blood pressure was over 160 and the same blood tests were repeated and came back worse, so they decided to do an emergency C-section that afternoon. By that point, I just wanted the baby out! If they had sent me home, I would have been a wreck.
A few hours later, my otherwise-healthy little daughter was born at 4 lbs 3 oz., which in metric/hospital terms translates to 1899 grams. At our hospital, all babies born under 2000 grams (2 kg) go straight to the NICU, so… there we were.
The NICU [pronounced NICK-you]:
Neonatal Intensive Care Unit
Because I’d just had a C-section, I wasn’t allowed to follow my baby to the NICU immediately. In fact, I wasn’t allowed to leave recovery until I could feel my legs, and at that point, they were nowhere to be found.
I absolutely hated the feeling of the spinal anesthesia; I didn’t want one at all during the delivery. The fact that I couldn’t feel my legs was scary enough, but the idea of my tiny, helpless daughter being taken alone to the NICU made me want to cry. What if she was scared? What if she wanted to hear the voices she’d heard for 36 weeks? I made a decision, which turned out to be a good one: I sent my husband with the baby. This might not be the choice for everyone, but my only concern at that point was what would happen to our baby.
I knew I’d be fine, and what could my husband really do for me at that point anyway? My husband followed the nurse to the NICU, with their permission, and was able to stay with the baby.
It was almost laughable to me that all our Lamaze training had completely gone out the window, as we were planning to have a drug-free and pain-free (I know, ha!) birth. Instead, here I was with an IV in my hand, a catheter in my you-know-where, and completely unable to feel the lower half of my body.
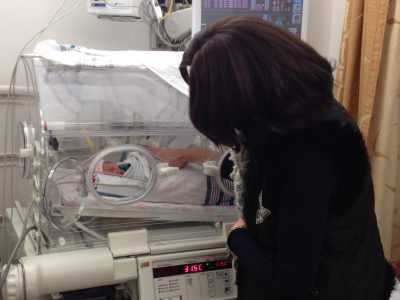
Non-critical NICU admissions seem to follow the same pattern: The babies are cleaned, assessed, and put on little warming trays. Then, in most cases, they are put into the ever-present incubators (below).

After about two hours, I could move my legs (yay!), and I was technically allowed to see my baby. Unfortunately, in my case, I had what they called “positional nausea” as a reaction to the C-section anesthesia. What this means in plain English is, “throw up when you sit up.” They wheeled me to the NICU on a stretcher to get a quick look at the baby, I sat up and… yeah, you get the idea. I came back much later that night when my anti-nausea meds kicked in.
My daughter was in the NICU for ten days, four of which I was in the hospital with her. Her 10-day stay also included a bout with newborn jaundice, which is extremely common and even more so for small babies.
Thankfully our NICU story has a very happy ending, as she’s home with us now and weighs almost 8 lbs at 6 weeks. However, the NICU road is always bumpy, whether your baby is in critical condition or just needs to grow a bit more.
I compiled this list of what I hope are helpful hints, in case any of you find yourselves in the same boat.
Tips for NICU Parents — How to Survive
1. Be a presence. Make yourself known. Introduce yourself to the doctors and nurses and even to the orderlies and desk attendants. Make sure they know which baby is yours. It’s human nature to feel more accountable if one is feeling accountable to a tangible being (i.e., you). You want the medical staff to know that “Baby Girl H.” has actual parents who will want to keep up on her progress. The best decision we made was to have one of us there for the doctors’ rounds each morning so we could meet with the actual doctors and discuss our daughter’s progress. But, that said…
2. Do not move into the NICU. Your baby is likely in an incubator, which presumably reminds him/her of exactly one place: the womb. The temperature in an incubator mimics that of the womb, and smaller babies are even given eye coverings. YOUR BABY WILL NOT KNOW IF YOU SLEEP AT HOME OR KEEP BEDSIDE VIGIL. So please, go sleep in your own bed, whether during the day or at night. If you’re still in the hospital, return to your room. Trade off shifts with your spouse if you wish, or go there together a few times a day. But make sure to ground yourself in your own house or room. Look at it this way, you are getting something few postpartum mothers get: time in your own home, your own shower, your own bed, and with someone else caring for your baby.
Spending at least a few hours a day on your own turf will make you feel like yourself again. After all, you’re not the patient anymore — your baby is. He needs you to be strong and clear-headed, whether to relate to him or to advocate for his care. If you let yourself get run down during this week (especially after a C-section), you’ll be in no position to care for him when you need to. Some mothers resist this because they don’t want their babies to bond with the nurses instead of them.
Admittedly, I was one of these mothers at first… but trust me, this won’t happen. First of all, your voice and smell are intimately familiar to your baby; he’ll know who you are. Second, there are many people who get ‘night nurses’ for their babies at home; this is no different. Third, and most important, if you’re sleeping at the hospital while your baby is in an incubator, how are you bonding with your baby at that moment? You’re not. You’ll be there when you’re awake, and if your baby needs care in the meantime, he’ll have a world-class staff available.
3. Eat. Sounds simple, right? But between shuttling back and forth to the hospital and sleeping, or not liking the hospital food, eating may fall by the wayside. Bring your own food to the NICU if you need to. Ours had lounges and a “no food in the rooms” policy… but let’s just say the nurses always looked the other way when I took out my bagged breakfasts and lunches in the baby’s room. If you’re nursing or pumping, you’ll need the calories even more.
4. Accept offers of help (and ask for what you need). If friends offer to make dinner, say yes. Don’t have friends offering? Perhaps your church or synagogue has a group that does this. Retract the orders for your mom to wait to visit until the baby comes home. If you have other children, send them to a friend or relative’s house if you need to. Accept rides to the hospital if you can’t yet drive. I was surprised that many of my friends didn’t even know my baby wasn’t home with me; if none of your friends has offered to help, perhaps they just don’t know what to offer. So tell them.
5. Familiarize yourself with your baby’s care and don’t be afraid to ask questions. If you have no medical background at all, the array of monitors and medical terms can be confusing. If the nurse tells you that “his pulse ox is 96” and this sounds like a foreign language, stop the nurse and ask what this means. What’s pulse ox? What’s normal? Don’t be afraid to advocate for your child. “I know you’re telling me that my baby needs formula tonight, but I always thought breast milk was best. Is there any way we can try nursing too? Or is this just temporary?” Along with this is…
6. Don’t be afraid of your baby. Many new mothers are afraid they’ll ‘break’ their little ones; this anxiety increases tenfold when your little one is tiny and/or hooked up to monitors. Be assured that the nurses would not let you handle your baby or leave the room if they didn’t think she could handle it. In fact, most NICUs encourage “kangaroo care,” which consists of putting your undressed baby on your bare chest for skin-to-skin contact. This is of great benefit to the baby, and again, you would not be given the opportunity to do this if the baby were not well enough.
On a touchier subject, I know some NICU parents hesitate to talk to, sing to, or otherwise bond with their baby because they’re worried things won’t work out. But even if your baby is in critical condition, the talking and singing will help him. It will help you as well; you’ll feel more connected to your little one and you’ll both be in a better position to fight and struggle as you need to. Look at it this way: if you distance yourself from the baby at this time, you may end up regretting it no matter what happens.
7. Take advantage of the education offered. At our NICU, the nurses were extremely focused on parent education. We learned how to feed, burp, change and bathe our little one. We took her temperature each hour and (sorry) learned what normal stools looked like. Everything. I’m very grateful for this; sometimes I even wish I’d taken some phone videos! The nurses are there to show you what to do; don’t be afraid to ask them.

Back at Home
When my baby came finally home, I expected my NICU experience to be a thing of the past. Strangely, though, several elements followed me home. I’ve given these trendy faux-medical names:
1. Post-NICU guilt. Here’s how this one will turn up in your head: you’ll find yourself thinking things like, “Since I didn’t hold my baby much during the first ten days of her life, I must now pick her up at every whimper.” Resist this. This might be enjoyable at first, but trust me: it becomes less and less enjoyable. Your baby is now home with you; anytime he needs something, you’ll be there. But if he needs to learn to sleep on his own or suck on a pacifier, now is the time for that too. Your baby is now able to have a normal home-life, and that should come with sleeping in a crib/bassinet/whatever you’ve chosen.

2. Post-NICU monitor anxiety. Some babies come home on monitors; if this is your case, skip to the next tip or apply this to the non-monitored functions. But if your baby does not come home on monitors, this one presents as follows: “My baby has been hooked up to monitors since he was born; now, how will I know if anything is wrong?” You’ll know just as mothers throughout the ages have known: crying, a fever, or something just not seeming right. Here’s a fun fact: did you know we all have to catch our breath after we sneeze? Do you want something beeping and flashing red every time your baby sneezes with no nurses around to explain things? Right.
3. Post-NICU medical worry. Here’s this one: “Her temp went down .1 degree one night in the NICU and they gave her an extra blanket. Maybe she’s not ok enough to sleep in this new onesie my sister sent.” Repeat after me: teams of doctors have unequivocally determined that your baby is ok enough to be home. If the hospital has given you discharge instructions, of course you will follow those; but in general, babies will not be home if they can’t maintain their body temperature in a different onesie, for example.
4. Lack of faith in your “regular” pediatrician. “In the NICU, they told me to give 30 ml of formula every three hours. She’s hungry every two hours now and my pediatrician said it’s fine. But I mean, he wasn’t there, so maybe he doesn’t know..?” Part of medical care, and especially critical care, is physician follow-up. Your pediatrician likely visited your baby in the NICU, and if not, he’s spoken to the doctors there. The NICU medical staff was giving you instructions for your baby at that moment. Now your baby’s doctor is his normal pediatrician, and his advice now is just as appropriate as theirs was then.
In short – your baby has started his life as a critical care patient. If he’s still there, he’s in very good hands and is receiving the best care possible. If he’s home, he’s now well enough to follow the track of non-critical babies. Now, he can grow, eat and sleep in your house. Either way, keep yourself healthy and clear-headed enough to take care of him, and you’ll both be better off.

Thanks for this helpful piece. I just delivered my 32 week old baby 2 days ago and your post made me feel a lot better. Thanks for all of the great stuff, Lucie.
I had just the opposite prbeolm with my daughter. She was born normal and healthy, but I was the one in ICU for 3 weeks after she was born. I thought she wouldn’t even know me, and that she wouldn’t like me. I had all the same feelings you do. But your child will know you the minute you are able to take him home. He’s heard your voice for 9 months, he knows you and he knows who you are. He’ll bond with you as soon as he’s able. Jaundice is OK. Most babies will get this. They can fix it, so don’t worry. Also, your motherly hormones are kicking in, you want to be with him, and you can’t. You worry more about this than he does, I promise. I held my daughter maybe 3 times in her first 3 weeks of life. Once I got home from the hospital, she took right to me. She knew me, and your son knows you, too. He just has to get better first, then you can hold him all you want!!
Thank you! Boy did this topic come through at the right time…as I lay on bed rest, 33 weeks awaiting the early arrival of our IUGR baby. Just what I needed to read at this time to help me come to terms with and understand what we are preparing for. I’m glad everything went well for you and your baby.
This article comes at the right time! A week ago I had my IUGR baby at 32weeks. She’s in the NICU doing very good and with no complications so far. I love to read “been-there-done-that” moms stories because they make you feel that you are not alone!
I agree, kangaroo is the best thing to do and even for the mom, makes your mood change! Before, I entered the NICU crying just seeing my baby girl surrounded by wires and tubes, looking so fragile! Now, after I’ve hold her many times, I’m happy to enter the NICU and just interact with her!
Thanks for this article Lucie!
I just read this in my weekly email update while I am currently having one of my twice a week NST’s. My baby is IUGR (7th percentile), they have known this since I was 27 weeks and I’m 33 now. Hoping to make it a few more weeks, and I’m not on bed rest. I go to one of the best hospitals in the world and it has a brand new nicu with 47 PRIVATE rooms for each baby’s incubator with a pull out couch for a parent to stay. Hopefully if my little guy makes it to week 37 he won’t need to stay long. I’m an RN so I’m a little more comfortable with all the procedures and equipment even though this isn’t my specialty, but reading your story was still very helpful. Thank you!
I’m 33 weeks, and I found out 1 1/2 weeks ago my cervix has shortened. Doc said I’m 50% effaced and 1-2cm dilated. I’m not on bed rest, but I’m trying to take it easy. I’m not sure if I should be worried about preterm labor or if my case is actually pretty normal? I’m a new mom and pretty terrified!
This article could not have come at a better time for me. My water broke at 31 weeks and I have been waiting in the hospital trying to keep him inside. Yesterday the doctor said that they will deliver my baby between 34-35 weeks, which means he will spend time in the NICU. Being in the hospital, we have already toured the NICU and spoken to the doctor but the mom in me is always guilty and worried about the baby having to start his life there. I will try and hold on to your words as encouragement.
Good luck to you! Stay positive. Have you checked out keepemcooking.com?
Great read! Thank you for posting information about this. I’m at week 33 and due to having a loss at 9 months last year, my doctors are talking about induction and possible time in the NICU. This was incredibly helpful.
This is a great article, even reading the comments is encouraging. My baby was recently diagnosed with rh disease, which puts him at risk for a stay in the nicu once he is born, whether he comes early or not. The dr wants to induce me by 38 weeks, so I am hoping that he decides to come on his own sometime before then. My first pregnancy and birth went so smoothly, I never thought I’d be reading info on complicated births and how to survive the nicu.
I’m 33 weeks as well and dealing with IUGR. Baby is 3 lbs. and in the 10th percentile. We were told they would induce and take her out if she reached that point, but all other signs look good so we’re going to keep her in a bit longer. It’s worrisome to know she may not be getting the nutrients she needs, but all I can do is monitor movement and make sure I’m getting enough protein and rest. We toured the NICU last week, which was a great experience. The staff was very reassuring and even showed us a baby about her size.
I’m 32.5 weeks and baby was just found out to be in the 9% for growth, weighing 3lbs 11oz. They increased monitoring from here on out and I’m trying not to freak out. Your article came out at a good point and makes me feel better!
Thank you for this (while I sit in my chair in the NICU pumping)!
I so wish I would have received this post two weeks ago. I delivered at 31 weeks due to severe pre-eclampsia. My little one was 3 lbs 1 ounce and is still in the NICU. The first couple days were the hardest because it was emotionally taxing to see her tethered to all the tubes and leads. I think your article is pretty spot on. I would add one piece of advice which I’ve learned over the past two weeks, do what is best for you and your situation. Just as it is important for your baby to get healthy, it is important for you to be healthy. This might mean missing a feeding to take a nap at home. Do what is best for you, it will go a long way.
So interesting…. I am in the hospital at 33 weeks today and received this email. I have 2 other children that were full term, vaginal births and great pregnancies. Im admitted because of contractions. So many things running through my mind. C sections are scarey, not being able to hold my baby or breastfeed has frightened me. Possibly going home without her is unimaginable. Thank you for the extra comfort with your email. Glad to say this is not her time to come and we are going home!
This was so helpful thank you! It came on the day that I was told about IUGR for my 31 week old baby girl. I’m hoping she will stay in there to term but this is helpful and reassuring and thank you for all the comments as well.
This is amazingly timed. Just yesterday I was sent to be admitted to labor and delivery to monitor my baby at 32 weeks and 6 days. Today I’m 33 weeks and officially told the baby is IUGR and I recieved 2 steroid shots along with magnesium. I’m terrified of what might happen and of the csection but reading this made me calm down a little bit knowing yes things can go wrong but look at what will most likely happen. Thank you
I would like to see more articals like this. My water broke at 30 weeks, and I was on bed rest in the hospital till my son was born at 31 weeks. (The goal was to make it to 34 weeks before they induce me.) He is 3lbs and 5oz and in the NICU as I write this. It has been 2 weeks and we continue to go every day if not two times a day. Each time it’s harder to leave because you bond with your baby. However the NICU is the best care they can get.
I agree withy the other moms. You do have to go home and sleep in your own bed. That is the only way you will regain your strength. Unfortunately there isn’t a ton you can do until he starts breast feeding. Your baby does know your voice but they don’t always know if you are there or not.
Is there a baby carrier (the kind you strap to yourself and hold the baby in) that is made for preemies who will weigh about 4 l/2 lbs when he leaves the hospital? Most I’ve looked for are for 8 lbs and up.
Hi Judy! Great question 🙂 First, you should definitely consult your pedi before using any babywearing apparatus. Once you’re given the go-ahead, We really like the Boba wrap and the Kangaroo Tube.
Thank you! This helped ease my mind. I’m a first-time mom and at 33 weeks I am being monitored for low amniotic fluid. If it doesn’t get any higher and is causing our little girl stress I will have to deliver early.
Our baby had to be in the NICU far from home, so we had to stay at the hospital and live out of my hospital bag. While the staff can be great, they can try to intimidate you into doing things their way or the easy way for them.. Since we were at the hospital, I said I would breast feed WHENEVER needed. They really tried to get me to gove him formula or supplement with formula. I compromised and let them give him some donor breast milk. They wanted him to have a pacifier and I would find one in his mouth even though I told them no. They wanted to do another CAT scan and I told them no he had had one and they said he hadnt, but when they dug deeper, they saw that he had… Bring a notebook and pencil and track EVERYTHING. Times you see him, what nurses were there, any procedures or medications..
This is great timing! Our little guy was delivered via C-section on Feb 28th at 28 weeks 4 days due to severe IUGR. We were considered high risk & being closely monitored due to losing our first daughter at 32 weeks, but we had a second daughter with a completely uneventful pregnancy & no complications. Our little guy weighed 1 pound 13 ounces and was 13 inches long at birth. Now, 2.5 weeks later, he is already 2 pounds 6 ounces & doing well in the Vanderbilt NICU. We have a long way to go on this journey, but we have faith that he will be coming home. Reading these tips is so helpful – thank you!
Sitting the NICU with my now 33+1 baby (born at 32+1) and this has been helpful! I just woke up from a nap in the hospital chair but I have been sleeping at home at night. The take home tips are going to be so helpful for me!!
Great advice. I wish I had read it back in Oct 2014 when I had our daughter. We had a very similar situation as you, IUGR at 35 weeks, delivered at 37 via C-Section because she was also breach. Fortunately for us our 4lb 13 oz baby was only in the NICU for a few hours the evening she was born due to temperature issues. I too sent my husband with her. She is now a 24lb 21 month old! Now I’m 35 weeks with constant growth check ultrasounds hoping that our little boy won’t have the same issues. If he does, we will definitely take this NICU advise to heart. Thanks for sharing your experience!
This article could not have come at a better time and definitely helped with my fears. Currently 33 weeks and our baby boy is measuring in the 14th percentile, and they have fears that my placenta is dying and not getting enough nutrition to the baby, along with very low amniotic fluid. We are doing twice a week NST’s then another growth ultrasound at 35 weeks to see if he has made any progress, if not we will be delivering him early, most likely c-section because he is breech. Praying he has a miraculous growth spurt in these next two weeks, but if not I at least feel more comfortable about his stay in the NICU if it comes to that. Thank you!
Thank you so much for the take home tips! My baby is 3 weeks old today, born at 30 weeks, due to me developing preeclampsia. She’s been in the NICU this whole time and doing great!
So glad to hear! Congratulations!
Thank you so much! At 33 weeks today, we’re still doing so-far-so-good, but this is the most positive and comforting thing I’ve read about the possibility of needing NICU care. I feel like one potential worry had just dissipated. And with so much on my mind right now, that’s a major win. I really, truly appreciate you sharing this story.
This is a great article – I delivered at 28 weeks to a 2 lb 12 oz baby boy. One thing you don’t touch on in your article that I think is important is being able to identify symptoms of postpartum depression/anxiety and PTSD – parents of NICU babies are much more likely to experience these things and it’s good to remind new parents of NICU babies what to watch for and how to get help. It’s been 5.5 months, and our son has been home for nearly 3 months, and I still wake up from nightmares about my experiences there and experience extreme anxiety. It was 3 weeks after we were home before I felt sure that the NICU wasn’t going to call me to tell me they made a mistake and I needed to bring him back (funny now, but the anxiety wasn’t funny at the time). Great article with important advice, but this was one area that may have been lacking. I’d also encourage all parents to consider utilizing a Ronald McDonald House if there is one nearby – some have Day Pass programs so that even parents who aren’t staying there can benefit from their programs (such as homecooked meals, laundry facilities, showers, and a support system) – we couldn’t have made it through our 85 day stay without them!
Thank you soo much for this piece. My water broke at 31wks 5days and I had been stuck in the hospital for 2 weeks. I will be induced at 34 wks and my baby will have to go to the NICU. This is the hardest thing to think about especially if you had a normal pregnancy. This really helped me feel more calm and knowing that my fears are not unwarranted and I am not alone make it easier to deal with. Our tour of the NICU was a bit scary but I know my little one will be in good hands and I will definitely make my presence known. Looking forward for this part being over and bringing home a healthy baby soon.
Positive thoughts for you and your baby! — Meg
Thank you SO much for posting this. My first baby was born 6 weeks early (while we were on vacation..) and needed to stay in NICU for 8 days (while we lived in a hotel). Though he’s a happy, healthy 2 year old now, it was pretty traumatic because we were just so unprepared and didn’t even know what NICU was. This is great and much-needed education for moms who deliver early and I’m really glad you’re putting this out there!
I’d also add, bond with the other parents in addition to the nurses. Whether you are there for 8 days or several months, having other people who empathize with what you’re going through can be really wonderful support.
That sounds hard that you couldn’t follow your baby the NICU. That sounds hard. My wife has been having complications, so I appreciate your thoughts on this.
It was a good read. Thanks for posting this.
Thank you for sharing your story and these helpful suggestions! It does this mama-to-be good to have this info as I prepare. I’m so happy your daughter is healthy and home with you!
This is very helpful, thank you! I’m in the hospital awaiting a scheduled caesarean for our little girl, who is nearing 33 weeks and weighs around 4 pounds. I was diagnosed with vasa previa at 20 weeks, which was very scary, and they want to deliver her at 34 or 35 weeks. I’ve been in the hospital for almost 4 weeks now and am constantly being monitored by a great staff of doctors and nurses. It’s our first birth, definitely not the birth story we had hoped for but I’m learning that no pregnancy goes exactly as planned, and every day with this little one has been a gift. Appreciate hearing from others and learning what to expect when she goes to the NICU in 1-2 weeks!