Suriving Postpartum Anxiety and Depression … Twice

I could never have known at the time – after all, she was my first – but looking back, I can say with utmost certainty that I began suffering from anxiety and depression during my first pregnancy.
I can’t say I am terribly surprised. I’ve been prone to anxiety my entire life. As a child, I worried constantly about all the things I couldn’t control; as I grew older, worry turned to panic, which turned to general anxiety about … everything.
Even though I so badly wanted to be pregnant and have children, I couldn’t stop the worrisome thoughts from incessantly invading: What if I’m not a good mom? What if having a child wreaks havoc on my marriage? Will I ever have time to myself again? What will become of my career? How will I multitask my life?
And so on.

As my due date approached, I didn’t feel ready. I wanted to keep her in longer because I knew this baby would be way easier to protect and take care of inside as opposed to out.
When I asked my doctor if this was a possibility, he laughed.
Except, I wasn’t joking.
At 42 weeks when she still hadn’t arrived, my OB said the words I really didn’t want to hear: “It’s time to induce, Marissa. She needs to come out.”

And so, on October 23, 2012, we went to the hospital early in the morning to begin the induction. For some reason (read: naivete), I assumed the process would move quickly – that the doctor would break my water, the Pitocin would bring on contractions, and within no time we’d be snuggling our little peanut.
Except that’s not what happened at all.
The entire process, beginning to end, took 16 or so hours. Somewhere around hour 14, my OB explained that my labor process had stalled—I couldn’t seem to dilate past 7 centimeters—and since my baby was “sunny side up” (an expression that essentially means she was facing the wrong direction to birth vaginally), it was highly unlikely she was going to come out the way I’d hoped.
“Prepare for a C-section,” he said.
I started to cry.

This wasn’t what I’d envisioned at all. In fact, I had skipped right over the entire C-section chapter in my pregnancy book because I was so certain I wouldn’t need one.
When they finally wheeled me into the OR, I’d been in labor for several hours and had been battling a migraine and severe nausea for the past three. As they prepped me for surgery, I began vomiting, turning my head left and right so I wouldn’t choke. I was miserable.
The nurses and anesthesiologist were incredible and helped me survive the ordeal, but it wasn’t the beautiful birthing scene I’d so desperately hoped for. It was scary and a bit traumatic.
The whole time all I could think of was that when it was all over, I’d have a tiny human to take care of … and keep alive.

When the OB pulled my daughter out, I feigned elation. As he held her up in front of me and introduced her to me for the first time, I was angry at myself that I wasn’t crying tears of joy, or that I didn’t feel anything … except disconnection (from her, motherhood, and the entire birthing experience).

As the days wore on in the hospital – I wound up there almost an entire week – my fears turned to full-blown anxiety and panic, and my sadness transformed into hopelessness. Each morning when my doctor came in for rounds, I would burst into tears and ask, “Is this normal? Shouldn’t I be happy? Why am I so terrified? Why am I so depressed?”
“It’s normal,” they assured me. “You just had a baby and your hormones have plummeted. Plus, you’re recovering from a major abdominal surgery. It’s probably just the Baby Blues. In a few weeks, you’ll feel better.”
And so I waited.
I waited and waited and waited to feel better.
But I didn’t.
Weeks passed. Then months. Then an entire year.

And I didn’t feel better.
Some days I was able to fake it—to pretend that I was doing well and that I was really getting the hang of this whole motherhood thing—but anyone who knew me well knew it was a façade. I was falling apart inside and out. I was frazzled, not sleeping more than an hour or two at night (even after the baby started sleeping through the night). I feared leaving the house, because “we may get into a car accident,” or “I might slip and fall while holding her and she’ll get hurt, or worse…,” or “someone may try to kidnap her,” and so on and so on.
Type-A by nature, my obsession with schedules and my inflexible rigidity grew much worse. We absolutely could not, under any circumstance, bend my daughter’s schedule even by a minute. She had to have her bottle every three hours, on the dot, and she needed to nap at exactly 9 a.m. and exactly 1 p.m. every single day. And of course, she had to be in bed no later than 7 p.m. every evening—and if this got pushed late, even by five minutes, I was a panic-stricken mess.

Surely going to sleep late would throw everything off for days, maybe even a week, and then she’d certainly develop poor sleep habits, which would eventually turn her into a terrible student (because— hello!— she wouldn’t be able to stay awake during school), and, a sleep deprived disaster, she would likely drop out of school and wind up on the streets.
Gah.
It sounds crazy, I know, but this is how my mind was operating at the time (and, left to its own devices, still does…).
I call this “The Tumbleweed.”

The endless catastrophic thoughts just roll, and roll, and roll. The Tumbleweed grows bigger and bigger and gains more and more force, and before I know it, I can’t stop it. And so I follow along, and my heart races faster, my breath becomes shallow, my appetite diminishes, and sleep—oh, sweet sleep—becomes a distant memory.
I’ll never forget the evening my husband came home from work to find me curled into a ball, weeping on the floor. This was, perhaps, my lowest moment. I had alienated everyone—family, friends, caregivers, all the helpers—because I didn’t trust anyone else to take care of my child (read: follow all my obsessive rules and scheduling guidelines to an absolute T). Yet at the same time, I didn’t even trust myself to take care of her. I felt lonely, exhausted, and isolated, but I refused to ask anyone to come over and help so I could take a break.
I was a fragile shell of the dynamic woman I once was.
Everyone knew they had to walk on eggshells around me for fear of setting me off into a state of panic and tears. It was incredibly ironic that even though I was studying mental health (I was a marriage and family therapy graduate student at the time), and was particularly drawn to working with couples and new parents, I didn’t recognize the symptoms within myself or understand that what I really needed was professional help.
I honestly assumed this was just what new parenthood was supposed to be like – a terrible initiation, of sorts – and that I had to suffer through it to find my groove. I would even get angry with my husband when he suggested we get a sitter and take some time just for us; in my mind, this was a selfish notion because, as parents, we needed to take care of our baby—not a babysitter.
And yet the signs were all there.
I was in the throes of postpartum depression and anxiety. This perinatal mood disorder was clearly taking over my life and stealing all the joys of new motherhood from me. I finally realized this when I saw friends doing fun things with their spouses and children—things I would never have dreamed of doing, like going on vacations or taking day trips to the zoo—because it would have disrupted my daughter’s nap schedule or possibly made her (or rather, me) uncomfortable or nervous.
With support from friends, family, and most importantly, my husband, I found an amazing perinatal psychiatrist and a therapist who helped me work through the heavy torrent of fears, anxieties, and emotions. My husband was very encouraging, and he even came to several therapy sessions with me so he could learn how to best support me, us, and our family.
This made a huge difference for me – it showed me how much he cared, and that I wasn’t in this alone. Perinatal mood and anxiety disorders truly are family diseases—they affect and afflict the entire family system: mom, dad (or partner), and child(ren).
I remember feeling guilty for taking time away from the baby to finish my graduate program, to go to the gym, and even to go to therapy. I don’t know why it is that moms always feel they must put everyone else first, casting themselves to the back of their own priority lists.
When I voiced this guilt to my therapist one day, she said:
“You need to put your own oxygen mask on before assisting others, Marissa. If you’re not alive and healthy, you will be no good to anyone else. So take care of you first, and then you’ll be better able to take care of others.”
I don’t know why I’d never thought about it this way before, but her words struck a serious chord. In that moment, I switched my mind-frame and stopped looking at “me-time” as something to be ashamed of, or feel guilty about, but instead as my survival mechanism and the thing that would make me a far better parent, wife, and overall human being.
To this day, I preach self-care above all else—it is the most important thing a person can do for him/herself. People who don’t take care of themselves are usually unhappy and eventually always burn out.

I see that now.
After I sought help, my life improved dramatically. I grew much more connected to my daughter—she was no longer just a being to keep alive, but rather a beautiful, intelligent little person with a sassy and sweet personality.
My relationship with my husband grew stronger. The passion I once possessed, and that had completely dissipated, finally returned (I started writing again, working out, seeing friends, etc.).
In short, everything got better.
And then, when my daughter was two and a half, I became pregnant with twins.
TWINS!
Oh, damn.
I knew there was a slight chance I could get pregnant with twins because I was taking Clomid, an infertility medication that helps with ovulation. My OB had warned my husband and I that there was a 10 percent chance of conceiving multiples … but I really didn’t believe him (and my husband claims he never even heard the doc say this). Oops.
I’ll never forget the ultrasound tech’s words at our first doctor’s appointment:
“Oh look…There’s two of them! You’re having twins! I love when it’s twins!”

Let’s just say I was glad someone was excited in that moment. I looked over at my husband, and his jaw was open so wide, I could have stuffed a softball in there. And then there was me. I literally felt like I had been hit by a truck. I sat there, unable to breathe, salty tears streaming down my cheeks. All I could think was, “I can’t do this…I really can’t do this.”
The first thing I did when we got home that day was Google “how to come to terms with having twins,” because I knew that this was reality—there were two babies growing inside of me—and I had no choice but to get on board. Whether I thought I could do it or not, I was going to be a mom to a toddler … and twin babies.
Yet I couldn’t really stop the familiar fears from returning. The depression crept back in. The panic took hold. I worked through it fairly well on my own during pregnancy, but about six months after they arrived (postpartum depression and anxiety can occur any time during the first year postpartum), I fell into a deep state of sadness and despair.

There were days I simply didn’t want to get out of bed (but I did, because I had to), and felt that my family would probably be better off without me (I obviously wasn’t capable of taking care of three kids, and I certainly didn’t want my kids to see their mother this way).
It was around the winter holidays when the hopelessness reached its peak. One icy afternoon when I was driving alone in my car, I vividly remember thinking that if I “accidentally” swerved and drove off a bridge, it wouldn’t be so bad.

Whoa (right?)
The thought jolted me, and in that moment I realized just how far gone I was; I had never thought or hoped for something so morbid before. The postpartum depression had reached its peak, and I knew it was time to get help.
Again.
Because I was too overwhelmed with, well, life, my husband called my psychiatrist and therapist and got me appointments immediately. He took me to all my appointments, where I was put back on medication (I took—and still take—Lexapro. This may not be helpful for everyone, and that’s okay! But it has been exceptionally helpful for me), and able to start working through the feelings of futility and sorrow.

Within weeks, I began to feel better. But though relief did come much faster the second time around, each day of being “in it” felt excruciatingly long and painful. I remember waking up each morning thinking, “How will I ever manage to get through this day? How many hours until I can go back to sleep?”
During that time I lived on auto-pilot, doing what I had to to take care of three kids. I backed out of all social plans—my energy levels and desire to socialize were at an all-time low—and I would go to bed as soon as the kids were all asleep.
Today I am almost 20 months into life with three kids, and I am doing so much better. The smile has returned to my face—and it’s a genuine one. I am finding ways to carve out time for myself again, and I’m doing things I truly enjoy, like working, writing, exercising and simply breathing.

I will not lie and say that either recovery has been a cinch—both recoveries have been (and continue to be) a challenging process in which I still battle negative and worrisome thoughts—but I can say with confidence that I am truly healthy, happy, joyful and full of hope again.
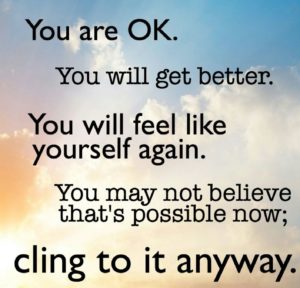
And so to any others out there (moms or dads!) who may be suffering from a perinatal mood and anxiety disorder, let me just say: You are not alone. One in seven women suffer from postpartum depression. This disease can take so much from you, but it does not have to defeat you. You can fight back, and you can win.
For every person who comes forwards and talks about her/his PPD and/or PPA and seeks treatment, there are several others who don’t. Let’s work together to eradicate the stigma around these diseases. There is help for PPD, and there is a cure! Please don’t suffer alone, or in silence. If you are struggling, please reach out for help. You are worth it!

For more information and to find resources in your area, check out Postpartum Support International.
How has a perinatal mood disorder affected your life? Please leave us a comment below.
Amazing work Marissa. I am always proud of your journey. Sometimes it takes some time to get through it on your own, then you have time to reach out to your network (who is always happy to help). Everyone does it in their own way, and that is perfectly fine. I am just so proud of you. Plus, when I see you at book club and Lifetime, I know you are back on track… go get it GUUUURL!!!
Thank you, Ali!
Thank you for sharing your journey Marissa. Speaking and sharing the stories of postpartum mood and anxiety disorders helps to encourage mamas to get help. We are not alone. Let’s find our tribe!
Thank you so much, Tory!
Thank you
such a wonderfully real read. I have a 14 month old at home and just found out we are expecting twins. I’m also on Lexapro and don’t believe I’d be here without it. Felt like I was reading a bit of my own story. Love reading about women who have been through it and came out on top. Well done Marissa
This is one I’m going to keep to share with students, supervisees, daughters of friends, my nieces, and perhaps someday my own daughter . Thanks for sharing your story with such openness and compassion. It’s a gift.
Thank you so much, Sara!
Thank you.
Thank you for sharing this. My son will be 3 soon. I went to therapy for 2 years and am doing much better but I still have bad days. Unfortunately, I had bad reactions to Lexapro and Prozac so I’ve had to make due with Xanax to manage anxiety and panic attacks. My father passed away in the middle of all this so it’s been an intense few years. I’m thankful for loving family and friends but to your point, no one can see how truly wrong you feel when you have PPD.
I applaud you for sharing your journey and being such a great mom of 3 wonderful children! Thank you for this write up as it really lifted me up today.
Chris, thank you so much for sharing this comment. I am so so sorry to hear how much you have struggled too, and I just can’t imagine losing a parent during the process. That’s beyond excruciating. I hope you are finding some peace and relief — you absolutely deserve it. Sending love your way!
I wish we were friends. You described exactly what i went through. The feelings. The thoughts. The actions. It took me almost 2 years to get help. And i have 5 year old twins. I never knew anyone before who could understand what i went through. And am still going through.
I am so sorry to hear of your struggles, Andi. I know what you mean – I wished so badly someone could relate and understand what I was going through. I most definitely get it! Sending love and peace your way! Oh – and cheers to being a fellow mama of twins (the struggle is real! :-).
Thank you for sharing your story. I also felt as if I was reading parts of my own story and birth experience.
Thank you so much for your comment, Jeanine. I am so sorry you have struggled too. Sending strength and peace your way!
Thank you so much for sharing your story. A lot of people still don’t understand or get it which makes getting through PPD/PPA more difficult.
I didn’t get treatment until my daughter was almost 18 months old. My husband was always against medication which was hard for me since I was a psych major and I knew I should have been getting help. Now I see a therapist, I take Wellbutrin and Zoloft, and take yoga a few times a week. I ended up going part time then leaving my job to be home.
It’s constant work to take care of your wellbeing AND someone else’s. I’m also pregnant with #2 which, as you know, has it’s own anxieties. Good luck to you and all others!!
Thank you for sharing your story. It’s very similar to what I am going through just now. I have a 5 year old daughter and 6 month old twins! I’ve just taken the step of seeking counselling for the first time. The realisation that I was struggling… my thoughts were heading in a very morbid way too. This was scary to admit to myself. I’m thankful to read your story and how you’ve made it out the other side!
Can you believe – I am in my 90’s and reading your experiences with PPD and PPA made my own seem like just yesterday. Yes, the weeping when you know you should be happy: the curling up in such distress and your husband not knowing what to do to help: the sheer despair and death wish – oh, such a terrible time! Back then (in the ’50’s) nobody dared to admit what they were going through for fear of being considered incompetent as a mother and so, you never heard about it from others.
Doctors seemed unable to help other than a pat on the head. There is more treatment available now and the best help is for new mothers to read a story like yours and to know she is not alone. There really is “light at the end of the tunnel” once you get those hormones
under control and joy to be found in parenthood. Thank you for your honesty and frankness.
Thank you so much for sharing YOUR experience here — enduring PPD and PPA at a time when it was not commonly talked about or socially accepted must have been excruciatingly difficult. But you’re absolutely right — the light at the end of the tunnel is real and there IS so much joy to be found in parenthood. Thank you for your comment!
[…] I’ve reflected often about my postpartum experiences, both after the birth of my oldest, and then after the birth of my twins. I’ve recently come to understand how dramatically this need for “doing”, “accomplishing”, “being perfect at”, and “never getting off the train” contributed (among several other factors, of course) to my two-time postpartum anxiety and depression. […]
[…] story goes on — I’ve written about it several times before, like here, and here. Postpartum anxiety and depression is a real […]
Thank you for this! I suffer from pregnancy postpartum depression and anxiety as well as PTSD. I took me months to get help after my daughter was born and like you said, I thought that’s what all moms go through. It was such a difficult and dark time. I too . couldn’t get out of bed and couldn’t eat; every thought went catastrophic. Reading your words definitely makes me feel like I’m not alone. I’m still doing therapy I medication 22 months later but I’m in a good place now and finally feel ready to have more children. Seriously, thank you. This meant so much to see another mom get through it.
Absolutely!!! You’re definitely not alone. Hugs to you, Natasha!
Thank you so much for sharing, Marissa! I relate so much… My postpartum depression turned into lifelong condition. My twins turned two and I’m still taking Lexapro. It was horrible during the first year and I was so afraid that my babies would be taken away if I told anyone what’s in my mind. After hospitalization and therapy, I realized that I’m not alone and I’m not my thoughts. Hope more people could see your experience and let’s try to remove the stigma around maternal mental health issues.
Hello, Lisa! Thank you so much for writing and for sharing your experience. I’m SO sorry for all you went through, and I’m also so happy you were able to get help and feel better. I totally relate to the feeling of being worried someone would take away the babies… it’s awful and so emotionally painful. Sending you so much love, and I’m with you 100 percent — let’s decrease the stigma. xo