Chances Are: Evaluating Re-entry Risk for Young Families

When I watched the Erin Burnett interview of Maura Lewinger, whose husband had just died of COVID-19, I cried along with her. This was back in April — the early days — when COVID was ravaging New York City. Here he was, a presumably healthy 42-year-old-man with a wife and three kids. A beloved assistant principal and community leader. Someone exactly my age.
Dead.
In that moment, one thing was certain to me after watching that interview: we were all going to die.
I watched the rain stream down the windows of my home office, a place where I’ve spent way too much time since then, and became immobilized with fear.
Anecdotes like this one are powerful. I mean, when your neighbor’s cousin who knew a guy who got sick and died, it really sticks with you. It’s a real story that happened to a real person.
My husband, a math and stats guy, calmly reminded me, however, that these isolated data points (i.e. the gut-wrenching stories on the news) are not representative of real data. After all, a story about a random person who survived – or even just had a mild case – doesn’t make for exciting news.
Media companies desperately need clicks to generate ad revenue in their struggle to stay afloat. You get more clicks by writing shocking and disturbing headlines, cherry-picking egregious cases and generally making things look as scary as possible. Everyone in the media knows this.
Just to be clear, COVID is scary. 100%. It’s freaking terrible. Perhaps you know someone who has died from it. But how scared should you really be??
As the weeks turn into months, and the devastation to the economy and to the mental state of parents and children becomes apparent, it begs the question: how do we proceed forward? Is it safe to go back to school/work?
Of course, the answer to this is different for every single family.
One thing’s for sure: nobody wants to get this disease. One forty-something friend described it as having glass in her lungs. No thanks. Also, there are still many things we still don’t know about it. Doctors agree that COVID-19 is a mysterious illness.
As we start to get our heads around what will or will not happen this fall, and many parents are faced with the daunting task of deciding whether to go back to work/childcare/school in person, it helps to really understand the actual statistics so you can logically think things through and make decisions for yourself and your family based on actual data for people like you (age, health, family composition, geography, etc.). So we put Brit, our lead researcher, to the task.
To summarize this article (tl;dr), the best candidates for going back to daycare/school meet the following criteria, more or less:
- Parent(s) whose livelihood depends on kids being in school/care;
- Children who don’t have any risk factors (obesity, heart problems, and other risk factors); the younger, the better (with the exception of infants under 1 year);
- Parents (under 50) of school-aged children who are healthy non-smokers with no risk factors and are not obese (being overweight or obese is a big risk factor in itself, but also a possible indicator of undiagnosed comorbidities);
- Families who do not have grandparents or other elders living in their home — or don’t interact with them regularly;
- The test positivity rate in your community is less than 5% (give or take), preventative measures are being taken, and your community is not 100% “open” (i.e. high risk businesses are not operating);
- Your child’s daycare/(pre)school is taking precautions to:
- decrease COVID coming in (temperature checks, questionnaires, preventing sick kids from attending);
- decrease possible transmission in the school: masking, distancing, keeping the kids in small, closed groups (where age-appropriate)
- rapidly identify any potential cases and responding appropriately (shutting down/notifying parents/etc.).
For more info on any of these, read on…
A big thank you to our friend Dr. Darria Long Gillespie, MD, MBA, who offered her time and expertise by way of an interview for this article. Among her many, many accolades, she’s an ER physician (trained at Yale), has an MBA from Harvard Business School, and has been featured on top-notch media outlets like CNN.
She’s also the national bestselling author of Mom Hacks, a mom of 2, and her instagram is packed with super-helpful videos for parents, too. In fact, this video (below) on back to school risk is a great place to start:
Living in a Pandemic
We’re now more than halfway through 2020 (what?) and nearing the end of summer, and it’s become more and more clear that we are a long ways away from any return to “normalcy” (whatever that means).
This is the news we all would prefer not to hear: contrary to what our current administration’s actions (or lack thereof) may suggest, we are going to be living with this pandemic for the foreseeable future.
And given that bleak forecast, I know I am not alone in wondering — what now? Because after those handful of brief moments when I’ve somehow mentally “escaped” (read: forgotten about) COVID-19, it all comes crashing back, and I think to myself: shit, I forgot to be scared.
Even with so much still up in the air, we do know more than we did a few months ago. And the trick with moving forward, it seems, is to try to find a new balance — some sweet spot where caution meets function. To try to act and live through a pandemic… sustainably.
*I think practically every parent in the US right now is wondering: how are we supposed to find that sweet spot for schools/daycare? Especially when the goal itself is a moving target, as evidenced by many in-person schools across the states being called off recently.
Thinking about school and childcare in the heart of the COVID pandemic is really complicated, but we’ve done our best to outline a mental map for thinking about back-to-school in the COVID era.
HUGE DISCLAIMER
This is not a guide or prescription for anyone. Our goal here is to bring you the current available data on the risks associated with COVID and introduce varying perspectives on how to approach the risks with schools and childcare so you can go forth and make a decision that’s right for you and your family — just like we do with all of our parenting advice.
And BTW — given how quickly things are changing, it’s easy for things to feel outdated in like, a day. Please know that we are doing our best to keep this page as up-to-date as possible, but also that our intent here remains to provide some structure for thinking about back to school even — actually, especially — in the midst of a shifting landscape.
With that lengthy and nuanced preface, here we go …
Is it Safe to Go Back to School?
I, personally, am desperately looking to the fall, praying to the gods of who-knows-what that my children’s preschool will please, please, pretty-please reopen (I admit) — but at the same time, I find myself wondering if I would even send them if it did.
So far, medical professionals and scientists studying the virus agree that, compared to adults, children are at a much lower risk for contracting, spreading and becoming seriously ill from COVID-19. More specifically, children (especially young children) are less likely to become infected, and it appears that infected children may also be more likely to have mild symptoms and less likely to spread the virus. (You can read more about this here and here.) The theory makes sense based on what we know about transmission — if you don’t have symptoms and don’t sneeze or cough, you are then less likely to pass the virus around.
That said, some experts, like Dr. Michael Osterholm, the Director of the Center of Infectious Disease Research and Policy at the University of Minnesota, also caution against putting too much stock in our current understanding of COVID in children (without contradicting it). We have to take these notions with a grain of salt, he says, because there is still so much to learn about COVID and we don’t want to risk getting “cocky” about things.
But it’s not entirely clear what all of this means for school: because no two schools or districts or families are exactly alike.
There is some promising data that suggests it is possible to reopen schools safely — although we can’t necessarily make widespread assumptions based on them.
Emily Oster, an all-star economist who also studies parenting issues, crowd-sourced information from almost 1,000 child care centers that remained open during or throughout the pandemic, serving roughly 27,500 students. She found that the average overall infection rate was 1.1% among staff members and 0.15% among children, respectively.
These data are not perfect, but they incidentally corroborate reports from some 1100 YMCA centers that provided child care during the pandemic for ~40,000 kids and never saw more than a single COVID case at any given location — including New York City in March and April, when the city’s disease spread was peaking.
Media reports of cases in schools in Texas have turned a lot of heads, however it’s likely that the overall rates of transmission there were small. Also, many schools and day care sites in Texas took few, if any, precautions to safeguard against COVID.
Outside the US, some other countries are reporting similar experiences to the YMCA — however many of them only reopened schools after having gotten COVID “way more under control” (hmmph) than is currently the case in the US, and they are not comparable to America generally (mask-wearing, testing availability, general belief in science, etc.). To use an analogy: here in America, the house is still on fire.
Looking abroad, Denmark saw no increase in cases after schools had been open again for five weeks (for children 2-12 years old); Finland and Norway reported the same; researchers in Iceland (where testing is impressively widespread among the general population) report that even infected children don’t seem to infect their parents. So did a recent study out of South Korea. Contract tracing projects abroad also failed to identify even one documented case of child-to-adult transmission.
Takeaway: Anyone can transmit COVID to anyone else, but young children (<10) are far less likely to spread it to adults — even adults living in the same home. And kids are more likely to contract COVID from their parents than from classmates. (But again, remember — kids are way less likely to contract COVID in the first place.)
Although school closures play a major role in flu pandemic response plans, there’s reason to believe that they may be less impactful in mitigating coronaviruses.
But still — we just don’t know how it will play out here in the US. When Israel reopened its schools, they experienced multiple outbreaks and had to close back down. Which reminds us, again, that as a country, we do need to understand that reopening schools will lead to some additional cases — it just will — and there’s no getting around that. (And some schools that have already reopened, especially in the South, have already seen cases crop up.)
Aside from these data and individual hopes (🙋🏻♀️), doctors, health professionals, educators and scholars have been increasingly expressing that reopening schools with multiple layers of safety precautions is truly an “urgent national priority.” Even the American Academy of Pediatrics released a statement in strong support of in-person schooling, wherever safely possible, come the fall.

It’s not just that working parents are in need of child care. Distance learning is replete with problems: millions of children have lost access to regular meals and health services provided at school; others are facing increased risks for abuse at home; underprivileged children are at-risk for falling behind; and American families are far from equally equipped to supervise the school day via Zoom. Not to mention the abysmal developmental and mental health effects children (and their parents) may suffer from the lack of daily socialization. I could go on… how much time do you have?
Of course, we can’t tell you — no one can — what’s going to happen with your child’s school, pre-K, or day care. Inevitably, everywhere will look different. (More on this in a bit…)
Although the administration is pushing (demanding?) for schools to reopen, it’s doing so unilaterally and blindly, without acknowledging the vast discrepancies in case rates and resources from one community to another; nor is it helping to empower local districts to make their own decisions or provide funding to enact the kinds of safety measures that would help them reopen safely (funding, manpower, etc.) As such, local school districts, health departments, education departments and individual care centers are all flying solo.
At the end of the day, every parent in America is anxiously waiting to hear what’s going to happen with schools and care in their area. After months of research, we’ve identified the 4 important questions you should ask yourself when trying to make the back-to-school decision (if that option is even available to you):
- What are your family’s needs?
- What are the risks for your family?
- How are things looking in your community?
- What precautions is your school/daycare center taking?
1. Your Family’s Needs
First and foremost, consider what you (and your kids) need or want to happen with school/care.
For some, this may involve a not-insignificant amount of soul-searching. Are you in desperate need of child care for work purposes? Or mental sanity (<< I count myself in this camp)? Did distance learning set off WWIII in your home last spring? Or did it go alright and you and your kids enjoyed the time? Or maybe you’ve always wanted to try homeschooling but never had the impetus?
Everyone is going to answer these questions differently — there’s no right or wrong here.
One third of American parents NEED their kids in school/care right now in order to work for a living.
For working parents, budgetary considerations vary depending on whether your child attends public school or private school/preschool, where annual tuition contracts are usually binding and payments are often due well in advance. For the latter, changing your mind midway through the year may be costly.
It goes without saying that your kids — their age, demeanor, temperament, everything — are also crucially important when considering the fall and school.
I want my own kids (who are 2 and 4) to go back to preschool because I know they are missing out on important windows for social development; because I know that their teachers regularly engage with them in more creative activities (and more patiently) than I do at home; and because I know they love it and miss it.
Though, I am also keenly aware that they do not “need” to go to preschool or daycare, and I wonder constantly about how and to what extent a socially-distanced classroom experience might impact their social development… And then I remember: kids are resilient. Not to mention — I can’t help but wonder if waiting it out a while longer could be the “better” thing to do for the greater good. But then again, I ask why parents should be asked to make these hard sacrifices and deprive their kids of a school experience when bars were so quick to reopen? BARS. I mean, what are our priorities, here?
As Osterholm asked: when our great-grandchildren write the histories of this pandemic, what are they going to say we did for our children?
Friends whose children are older have been very proactive about including their children in the decision-making process (much to everyone’s happiness). I know some people have even decided to move their family to a place that’s planning on in-person schooling.
At the end of the day, if you know you need school/child care in order to work, and you need to work to pay the bills, most likely, that’s that.
If you’re in the position of looking at school or daycare as a “choice,” start having conversations now about all you are wondering about. Chat with your partner or parents or school directors, your kids; write things down, and know that it’s OK to be unsure and/or to change your mind later.
As Dr. Darria reminded us, uncertainty is a fact of life right now, so it’s okay to be uncertain yourself. It’s okay to say “I don’t know.” For those of us who thrive on planning in advance, it sucks — we know. She reminds us: “just because we have uncertainty doesn’t mean we have to feel paralyzed. It just means that we need to think through different scenarios, so that if one thing happens, we can pivot – AND we can have more peace of mind knowing that we have plans in place.”
2. Your Family’s Risk
A huge part of thinking about going back to school is *trying to understand the individual risks — for you, your child(ren), and your family.
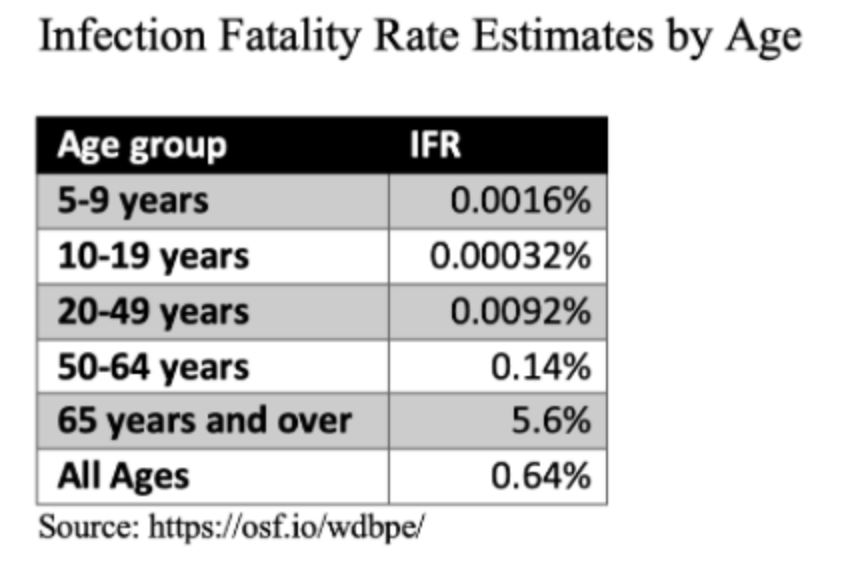
There is no single death rate for COVID (or any disease). Mortality risk for COVID-19 varies drastically depending on circumstances. The number one biggest variable is age (people over 65 account for 80% of deaths) Another huge one is underlying conditions (people with underlying conditions are 12x more likely to die). Another is race. Another is location. And timing (think about contracting COVID in April in NYC, when hospitals were in dire straits and ventilators were in short supply, as opposed to getting ill now, when many locales have enacted preparedness measures to guarantee more hospital and critical care access/supplies).
Put simply, the risk of dying from COVID-19 is highly stratified; it depends.
For Kids:
Generally speaking (and according to the preliminary studies out there), the younger a person is, the less likely they are to catch, spread, and become severely ill from COVID.
If you have a high risk child, you probably already know it. These conditions include children with medically complex conditions, children who are obese or morbidly obese, children with neurologic, genetic, or metabolic conditions or congenital heart disease.
Infants and Young Children
Dr. Darria says that we should consider babies (<12 mos) as medically vulnerable, simply because their immune systems are still immature.
Young children, aged 1-5, are probably the “lowest risk” age group from COVID: they appear to be less likely to contract COVID than adults, develop complications less often, and infect others less often. This should be an important fact for everyone thinking about day care, preschool, and even early elementary right now — although there are still many variables that remain.
All of that said, sometimes it seems as though the cards are changing every day, as new information comes out and the caveats are unending. Case in point: in early/mid August, the AAP released a new analysis concluding that 8.8% of US COVID cases occurred in children — though most states categorized children as aged 1-19. And a study released in JAMA showed that infected children under the age of 5 can harbor significant amounts of CV viral nucleic acids — though not necessarily infectious virus. Keeping track of it all is a full-time job in itself.
Keeping Things in Perspective
It’s hard not to obsess about coronavirus these days. It’s everywhere you look, everything you read. It’s every mask you see walking down the street and every “closed” sign you see in store windows. It’s (necessarily) a national obsession.
But… it’s always useful to step back for a minute to look at the big picture.
How often do you think about the risk of getting in your car every day? Approximately 339 kids die every month in auto accidents; 261 kids die every month from firearm accidents; and 82 kids die every month from drowning.
Thirty children (under 15) thus far have died of COVID-19 since the beginning of this outbreak in February; most of those children had chronic medical conditions. Our friend Dr. Darria reminded us in a recent phone interview that sending children back to school is not a zero-risk endeavor, which is why we have to be very vigilant as we move forward. But… we need to keep it in perspective. It’s difficult to talk about, because thinking about the death of a child as a statistic is totally misguided, but Dr. Michael Osterholm explains that COVID doesn’t even come close to being in the top 25 causes of death for people under the age of 24.
For Adults:
Let’s zero in on risk for the under 50 crowd (i.e. parents of school-aged kids). Again, age is in our favor. Even middle age.
After age, one of the biggest (and touchiest) risk factors for this age group is obesity. Dr. Darria told us that obese individuals have a 40% higher mortality risk from COVID (across all ages.) They also have a 75-80% higher chance of experiencing respiratory failure (according to one study).
To be clear, it’s not necessarily carrying extra weight in itself that puts people at high risk (though it can, see below). Rather, it’s the fact that being overweight tends to overlap with other comorbidities that are often undiagnosed at this age — namely: type 2 diabetes, hypertension and/or heart disease — and also increases the risk for serious illness and/or death from COVID-19. Carrying extra weight also tends to disproportionately affect disadvantaged and minority Americans who lack resources and access to health care.
“The news reports headlines like, ‘22 year old dies of coronavirus.’ What they don’t tell you is that person was morbidly obese with multiple comorbidities. That doesn’t make it ‘acceptable’ or any less tragic, of course; it doesn’t mean that it was that person’s *fault* — and it also doesn’t suggest that anyone else should be cavalier.
– Dr. Darria
However, we do have to keep in mind the full context because headlines like that really just have one goal — and that is to scare people and make them click on the story… it’s not at all to educate or empower the reader with how best to stay safe.”
One of the big problems with the “young to middle-aged parent” age group is that many who actually do have a health problem don’t know it because they aren’t old/sick enough to have been officially diagnosed with it yet. Whereas older Americans are more likely to have been formally diagnosed (and/or treated for) chronic disease, younger and middle-aged busy parents are not. Let’s face it, many of us haven’t been to the doctor in… a while.
Among Americans, 40% of adults aged 20-39 years are overweight or obese, and nearly 45% of 40-50 year-olds are overweight or obese. This means a lot of parents are at high(er) risk. And it seems to run on a continuum — for all its problems, we’re using BMI as a stand-in here, and the higher a person’s BMI, the higher his/her mortality risk from COVID. (Click here for a BMI calculator.)
“Research has shown that people who are obese often have impaired immune responses, meaning it is easier for germs like viruses and bacteria to invade the body and set up an infection. Being obese also makes severe complications from infections more likely, including acute respiratory distress syndrome or ARDS (one of the most serious symptoms of COVID-19), thanks in part to higher oxygen demands from a larger body.” (See also: The Covid Symptom Study.)
Why? Obesity can actually impact how a person’s lungs work, affecting the ability to breathe deeply and interfering with the mitochondria in their lungs’ lining. Adipocytes (fat cells) are also pro-inflammatory, which means they can contribute to numerous health issues, including blood clots and a “cytokine storm,” which is basically when a person’s immune system goes haywire — it kicks into overdrive and aggressively attacks the body’s own cells (they’re associated with COVID-19).
We were pretty shocked to hear one hospital administrator (a parent-friend) who studied COVID data in her system state her litmus test for making this decision so bluntly: “In looking at our hospital’s mortality data… if I were over 250 lbs (give or take, and depending on height, etc.), I would not be sending my kids back to school.”
Of course, outside of metabolic disease, there are other risk factors for adults under 50, but we’re guessing you probably know if you fall into this category. After age and obesity, Dr. Darria sees the next biggest risk factors as COPD, heart disease, kidney disease, and diabetes (in no particular order).
The good news? Managing a comorbidity can have a huge effect. Dr. Darria explained to us, for example, that just moving from being an “uncontrolled diabetic” to a “controlled diabetic” (meaning you’re being medically treated and actively managing the condition) drastically reduces a person’s mortality risk for COVID.
She says doctors see three separate risk groups for people whose age does not immediately put them at risk (<50):
- Low risk: a person with no diagnoses and who is not overweight;
- Medium risk: a person with a diagnosed comorbidity but who has the condition under control, or someone with a precursor to a formal diagnosis, such as prediabetes (the NIH estimates that a third of American adults have prediabetes);
- High risk: a person with an uncontrolled diagnosis (such as morbid obesity or uncontrolled diabetes).
We KNOW this is all a touchy subject. It’s uncomfortable to even bring up the topic of weight, but we think it’s an important consideration in helping parents in this age group understand their individual risk so they can make informed decisions.
Teachers
It’s impossible to mention the individual risks of reopening schools without speaking to the concerns of teachers, who have — very rightly so — come out in numbers over the course of the past few weeks asking why they should be asked to put their lives (and their family’s lives) on the lines. In Florida, teachers are suing the state government; Colorado teachers are petitioning the state governor; teachers in LA are demanding remote learning.
Teachers’ safety — and input — needs to be at the forefront of our thinking about reopening schools (not least because more than 25% of our country’s teachers have an underlying risk factor). What that means for any particular school depends, but one thing we cannot do is discount teachers’ very real concerns about their school’s abilities to safeguard teachers and staff as well as the implicit expectation that teachers must show up for in-person schooling.
Obviously, knowing the statistics can only take you so far. And “not wanting to die” is far from the only motivating factor with COVID. Obviously.
“Risk decisions,” explains Dr. Baruch Fischoff, “are never about one risk alone.” Making choices — with COVID-19, as with all things — inevitably involves weighing possible outcomes and thinking about trade-offs. If avoiding COVID-19 is your sole goal in life until there is a vaccine or a reliably effective therapy, then the safest way to achieve that goal is indeed to stay home. And to keep your kids home, too.
But for most of us, in real life, avoiding COVID is not the only consideration. We have families. We have jobs. We have life to attend to.
COVID is not a black-and-white yes/no situation — it’s more helpful to think about the risks as being on a spectrum. “Everything’s a trade-off,” Dr. Erin Bromage explained in an interview.
Dr. Darria likens thinking about COVID to talking to her 6-year-old about the ocean: “We have to respect the ocean,” she says. The idea is this: we don’t need to be terrified or paralyzed by the ocean, but we have to be smart around it and protect ourselves from the real danger it can pose. COVID is the same: we shouldn’t be panicky about it — but we have to be smart, we have to protect ourselves, we have to respect it.
All of this is to say: part of the thought process for back-to-school involves trying to gauge your own family’s risks. There are basic health considerations (^^), as well as situational factors. If you have a multi-generational household, that’s obviously a huge factor. If someone in your family is an essential worker, health care provider or a first-responder, your perspective also may vary from that of a family in which one or two parents are able to WFH moving forward.
At the end of the day, if your household is fortunate enough to be relatively young and in relatively good health, it’s important to remember that neither youth nor age guarantees an “easy time of it,” but perhaps it’s reassuring to know some of the real data — and use that in your decision-making, as opposed to misleading (or alarmist) media reports that tend to skew the facts.
3. Community Transmission
Schools are not islands isolated from the communities in which they exist. As Dr. Osterholm said in his podcast episode on reopening schools, we have to expect that kids are going to get infected — because what happens into our community will spill into our schools.
Our nation’s numbers are all over the place. Some states look to be improving, while in others, case counts are rising sharply. Point being: every state and county’s situation is different.
At the outset, you can look at whether case counts in your state are rising or falling. The New York Times state-by-tracker is easy to follow.
Another thing: if your state’s case positivity ratio — that is, the proportion of tests that are coming back positive — is holding steady at between 2 to 5%, this suggests that your state probably has a decent handle on where COVID is lurking. A higher positive test turnout, though, indicates that your state likely isn’t seeing the whole picture (meaning, there are likely MANY more positives than what’s being reported) — this is reason to be more cautious. You can check your state’s status here (thanks, Johns Hopkins).
I keep thinking about what an infectious disease epidemiologist at Boston University told Rebecca Onion over at Slate: when she and her husband (who is incidentally also an infectious disease expert) talk about school in the fall, what they care about most — more than any specific precautions their kids’ school promises to take — is the level of community transmission in their area. No one can know for sure what that will look like in any given area come Labor Day (or the months after). (And if our nation’s track record with the three-day holiday weekends thus far is any indication… wooph what a September it could be.)
On a related note, you might also want to consider how well-equipped your state is to handle a surge in illness, should anyone in your family get sick. Most state health departments or state CDC homepages are now providing information on available numbers of critical care beds and ventilators, for example (and this tool from the CDC displays the estimated percentage of hospital and ICU beds that are occupied in each state).
Lastly, although there’s no exact science to it, Dr. Darria says it’s also worth thinking about the extent to which your community is currently reopened. As she explains, if everything else is 100% reopened, then reopening schools may put things over the top. On the other hand, getting kids back into schools in areas where things are only, say, ~70% reopened may be “less risky.” (Another reason this is important relates to protecting teachers, who worry that if kids can be fully “out and about,” they will have more exposure.)
4. School/Child Care COVID Precautions
You also want to know how your school(s) plan to protect against the spread of COVID and potentially adapt and handle any number of COVID-related issues. What will the new sick policy look like? The days of sending your kids to school “with a sniffle” are (hopefully) over. What will happen if a case is detected?
Dr. Darria says that the most important things are that the school is actively working to:
- decrease COVID coming in;
- decrease possible transmission in the school; and
- rapidly identify any potential cases and plan responses for various scenarios.
Here are some protocols many daycares and schools are considering, most of which can and should vary depending on age. When I think about physical distancing “happening” among teenagers in high school vs. among toddlers at my kids’ preschool, it’s drastically different (and I’m not sure which is more/less unrealistic… or useful):

Note: For children under ten — these measures are far more important for protecting adults (teachers and staff, parents) than for children.
- Developing and/or extending viable outdoor learning spaces, since outdoor transmission is relatively rare (the feasibility of this varies by location and by season — NYC is especially having trouble developing safe outdoor learning spaces for young children, for example);
- Outdoor drop-off and pick-up (and no parents in the buildings);
- Staggering drop-off and pickups at intervals;
- Temperature checks and symptoms screenings;
- Daily pre-drop off questionnaires asking parents to certify that children are symptom-free, and pose questions asking about known exposures or recent travel;
- Reduced class sizes (e.g. 12 kids with just one teacher);
- Schedule adjustments, including “hybrid options,” such as having children attend in-person school only 1-3 days/week, only in the mornings or afternoons, or every other week, and completing remaining lessons virtually;
- No classroom visits or transfer within schools (many programs are arranging “pods” or “clusters” that can interact more freely in-group but do not socialize with other groups through the day);
- Increased hand-washing and sanitary procedures throughout the day;
- Arranging desks/play stations farther apart;
- Mask-wearing (among teachers, and among students who are old enough);
- Requiring families to sign contracts agreeing to abide by certain precautions;
- More stringent illness policies;
- Students eating lunch in the classroom;
- No more field trips.
The AAP also lists age-specific policy recommendations for reopening, depending on whether your child is in pre-K, elementary school, or high school. Its policy statement further addresses transportation, communal spaces, and mealtimes. (The CDC also just released guidelines on reopening for K-12.)
For young children, reducing class size may be the most important and effective way to reduce the risk of COVID in schools (especially when paired with the “cluster” model). It helps limit the potential level of exposure, and, should anyone in the classroom become sick, it would also help facilitate swift contract tracing and potentially enable schools to continue to function (as opposed to having to shut down entirely).

Ideally, schools have a plan of action for if and when there’s a case, but just knowing a school has considered the possibility is more important than the details of its response. *More than anything, both parents and schools need to be flexible — they need to be prepared to encounter multiple different scenarios, be willing to change course, and know when to pivot.
To make problems worse, schools across the country are facing every kind of budget problem. Some schools and centers in wealthier areas (or with more governmental financial support) can make up for deficits and meet the need for additional expenses more easily than others. Other schools aren’t meeting enrollment minimums and may have to close altogether. It’s not a good situation, and it’s threatening to deepen inequality in an already-unequal school system.
By the way — it’s up to you to decide how you feel about COVID-related school precautions. Some parents want the whole gamut, all the safeguards. Others may see that as overkill or worry that the safety measures we’re relying on to protect our children may “taint” their childhoods somehow.
For anyone who’s reticent to have their young children to wear masks (guilty 🙋🏻♀️), Dr. Darria said that it’s actually a better strategy to get your child comfortable with a mask early on… AND to be a good mask model — meaning: wear one! Be positive about it! Yay! Kids are surprisingly adaptable (more than we are!). Just like technology, masks are going to be part of their lives and their youth, because, as we said, the COVID world isn’t going anywhere fast.
Summing Things Up
Expect this year to be a giant effin’ mess. Don’t worry about your kids falling behind — everyone will be “behind.” Don’t try to make it a “normal” year — it’s anything but. Do the best you can, and remember that everyone’s in a similar situation. I breathed a huge sigh of relief when Michael Osterholm suggested we approach this school year as “our COVID year,” because it felt like much-needed permission to just… breathe, and stop trying to force anything.
Eventually, we will talk about the pandemic in the past tense.
But for now, we are living in it.
So — to recap the technical details, here are the questions parents should ask themselves when deciding whether to send kids back to daycare/preschool/school:
- What are your family’s needs?
- Do you need childcare/school in order to pay the bills/stay sane?
- How do your kids fare staying home/going to school/care?
- What are your family’s risks?
- Do your kids have risk factors?
- Are you and your partner at low, medium, or high risk?
- Do you have elders living in your home?
- What is the community disease rate like in your area?
- Is the test positivity rate lower than 5% in your community (give or take?) Is your community “fully open” (bars and such)?
- What precautions are your daycare/school taking?
- Are children being broken up into smaller groups/pods where exposure is lower and contact tracing is quick and easy?
- Are children and adults using masks, shields, or other PPE?
- Will children be routinely checked for symptoms before arriving at care/school?
Just as with everything else — visiting grandparents, playdates, eating out, etc. — every family’s choices about school are going to vary depending on individual and situational circumstances.
School is a risk (sigh). And personal choices about risk are necessarily variable. We all don’t make the same bets. Especially not when the house is changing the odds every day.
On that note, I’d also like to say this: we are generally in the habit of making choices and then sticking with them (and thinking that such is the “right” way to go about decision-making). Especially as parents. But given that the ground is shifting beneath us each and every day, we will very likely be in the position of having to make and remake what feel like the “same” decisions multiple times over.
Anyways… the point IS: you will probably change your mind. A lot — and that’s OK.
Easier said than done… I’m still reminding myself of this^^.
There are no easy answers here, friends — only hard choices. At the end of the day, I loved what pediatrician Dr. Dipesh Navsaria conveyed to The New York Times about how to approach decisions that involve our children “getting out” in the midst of the pandemic: “I’m less worried about a parent or a business getting all the rules right, because we don’t know what ‘right’ is, and more concerned about them being intentionally thoughtful.”
This sounds within the realm of feasibility to me. Yes, we parents may not get it right every time, but damn, we can be thoughtful.
How are you thinking about back-to-school? Please join the conversation in the comments below — we’d love to hear from you.
I just want to thank the whole Lucie’s List staff for tackling issues that I care about in an informed, measured way. You never minimize the problems or risks of an issue, but you do provide fact-based resources and data that help educate me and allow me to put things in perspective on a myriad of topics. Your timing on sending out your emails is uncanny; you always know just when I need you most! This COVID-19 framework is no exception. I have deep appreciation for the work you do connecting parents to reviews, resources, and information that help us to make the best choices we can for our families.
Well said, Whitney L. I agree!
Thank you for putting this together. I know you put in a lot of caveats for “preliminary data”, etc., but some studies now apparently show that young kids may be even more contagious to their families than older kids. I’ll put the link below. So some of this may already be out of date unfortunately. It just shows how difficult it is to make decisions when this virus is so new and things are changing constantly.
“New Evidence suggests young children spread Covid-19 more efficiently than adults” at
https://www.forbes.com/sites/williamhaseltine/2020/07/31/new-evidence-suggests-young-children-spread-covid-19-more-efficiently-than-adults/#72a9736c19fd
Jennifer — Thanks so much for sharing this. Yes, it’s one of the (many) frustrating things that news about COVID can feel outdated in just a matter of days. We’re hoping that these key four questions will continue to help guide families who are thinking about school even through a changing landscape and rapid data turnover. I personally think the “back to school” decision is going to last this entire school year (at least) for most families.
Thank you for this article. I’m curious how the experts view pregnancy as a risk factor in determining whether or not to send your kids back to daycare – we have a 16-month old. If we don’t send her back to daycare next month, we’ll loose our space – or will have to continue to pay for enrollment with her at home, which isn’t financially an option for us. I’m currently in the second trimester of my third pregnancy and am otherwise at a higher risk to contract the virus because I have juvenile rheumatoid arthritis.
Thanks,
Jessica
Jessica — Wow this is such a great question (and I KNOW you are not alone), and it’s disappointing that there’s so little evidence (or even perspective) available on this. I’m sorry I don’t have much to help, but I’d definitely recommend speaking with your OB about your risk. Some child care centers are also being flexible with their standard tuition deadlines, etc., so maybe your care center would be willing to hold your spot given the circumstances (?). ACOG just updated its current statement on pregnancy and COVID based on a new report from the CDC, so that may be helpful in thinking things through. Best of luck with everything — we’re thinking of you.
Jessica — Not sure if you are still in the boat of deciding about daycare, but I just came across this post from Emily Oster, which discusses this difficult decision (scroll down to “Most Common Question: Pregnant with a Toddler”).
I really appreciate that you posted this. Thank you also for citing so much research and being clear-headed about the information. This analysis is very helpful for my brain and it helps unscramble some of the conflicting messages we’ve been hearing. I hope you will continue to update us as new research comes out; I think we’re going to be dealing with this for awhile!
Thank you for the attention you’ve put into this.
THANK YOU for writing this! Great approach and comprehensive review of what’s happening today
Thank you for this very thorough and informative article. You have truly done the research and have provided a very valuable blueprint of questions parents should consider when deciding what is best for their family. You make it clear that there is no single right answer, and depending on one’s particular circumstances, no one answer is a perfect fit. Thanks for providing your readers with great food for thought and giving us permission to feel alright about the decision we make for our family and our children, even if it is different from the decisions others make. The article also let us know it is okay to change our minds multiple times as circumstances evolve. There is no doubt this pandemic is ever-changing, and Lucie’s List had the courage to address this subject matter. Well done.
This is an unbelievable helpful and informative article!! Thank you so much for this. I am sharing far and wide. Fact-based, not fear-based. So so helpful.
This is the best summary I have read about the thoughts that have been swirling through my mind lately. I plan to share this with others in my life. Thank you!
well considered and great info- you continue to be a lighthouse in a storm for me since i had my daughter 4.5 years ago. THANK YOU!!❤️
a very well researched and helpful article, as a grandparent, thank you
@Jessica – I’d recommend Evidence Based Birth newsletter – they are sending out the latest research on pregnancy and COVID. https://evidencebasedbirth.com/covid19/
Thanks for sharing — another great resource is COVID Explained.
I’ve been a subscriber for 6 years now. You’ve walked me through registries, teething, breast feeding, sun are for infants you name it. Now at a soul searching difficult time for all parents… In walks Lucie’s list again! Your roadmap is the most calming thing I’ve come across and I had to stop reading Social media, as a parent and teacher it was freaking me out on a daily basis. Thank you for taking the time and effort to do this research and put this together!
What a wonderful article; thank you! I especially needed to hear the closing reminder that it’s ok to change your mind about this as things unfold. “Flexibility“ is one of my 2020 mantras.
This is so well done! Thank you for all the information you collected and put here. I just have one question – did anything about pregnancy/newborns come up in your research? I have two school age kids (preschool and first grade), an almost 2 year old and I’m due in November. I don’t work but I also have no family to help me besides my husband who does work. I’m seriously struggling with the decision of what is best for my kids and for the end of this pregnancy. I haven’t found much info yet myself.
Rachel — Thanks for your kind words! I’m so sorry that we don’t have much by way of help with this. We’re frustrated as well that it seems to be a huge void in the scientific and cultural conversations surrounding Covid. If anything comes up, I’ll be sure to note it here, though.
You all are the best so thanks for your hard work with this article! Lucie’s List is a wonderful resource!
Thank you so much for this thoughtful and informed road map to approaching this important decision. This has been such a hot topic in our household and this approach made it so much easier for my husband and I to have a productive conversation on whether or not to send our daughter to school. Thank you for always providing such helpful parenting resources – and for making me feel like I am not alone!